Understanding Sepsis and its Impact on the Body
Sepsis is a life-threatening condition that arises when the body’s response to an infection spirals out of control, leading to tissue damage, organ failure, and even death. This dysregulated immune response can be triggered by a wide range of pathogens, including bacteria, viruses, fungi, and parasites. As the body battles the infection, it releases a cascade of inflammatory mediators that can ultimately compromise the delicate balance of the circulatory and thermoregulatory systems.
One of the hallmarks of sepsis is the disruption of thermoregulation, the body’s ability to maintain a stable core temperature. Patients with sepsis often experience fluctuations in body temperature, ranging from fever to hypothermia. These temperature changes can have a significant impact on the body’s ability to fight the underlying infection and increase the risk of complications, including organ dysfunction and even death.
The Cecal Ligation and Puncture (CLP) Model
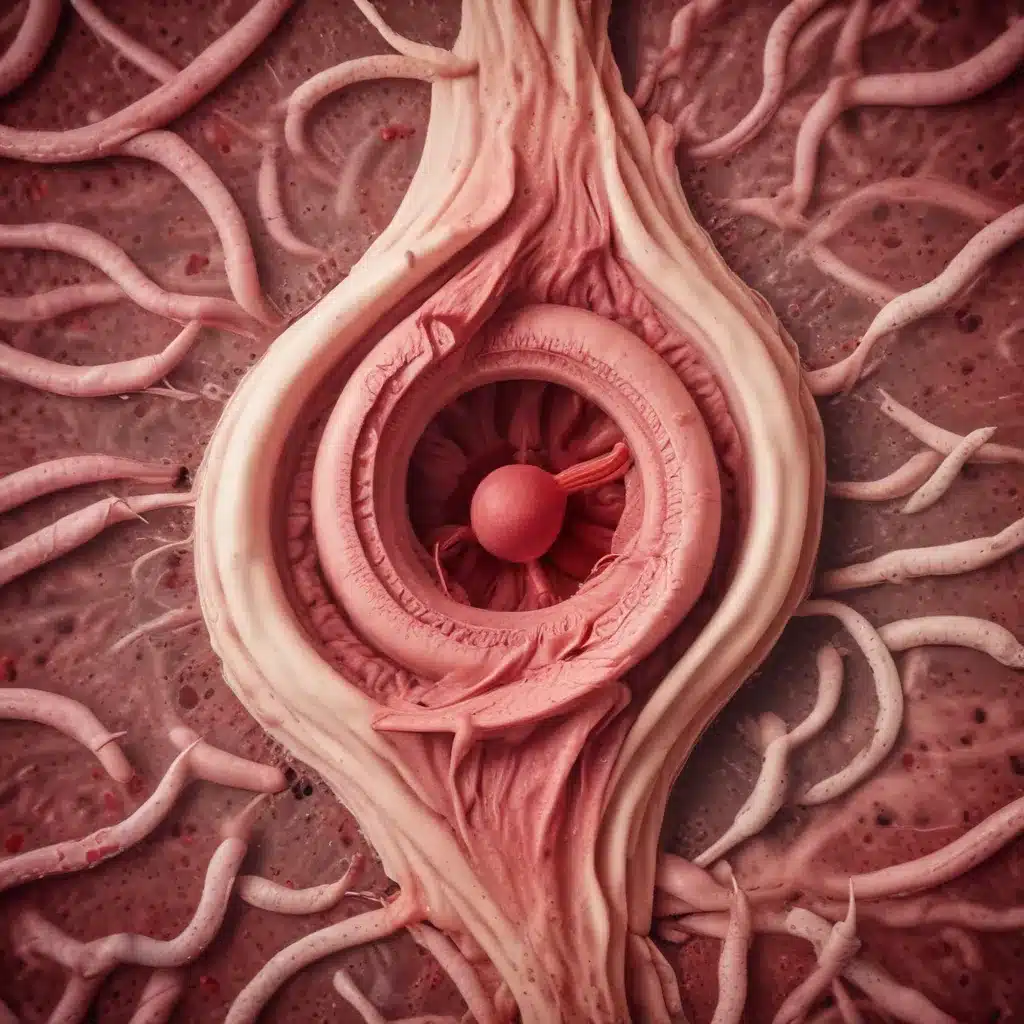
To better understand the complex interplay between sepsis, thermoregulation, and survival, researchers have developed the cecal ligation and puncture (CLP) model. This well-established animal model mimics the pathophysiology of human sepsis, allowing scientists to study the underlying mechanisms and explore potential therapeutic interventions.
In the CLP model, a small incision is made in the abdominal cavity, and the cecum (a pouch-like structure at the junction of the small and large intestines) is exposed. A portion of the cecum is then ligated (tied off) and punctured, creating a controlled and sustained release of intestinal contents into the abdominal cavity. This triggers a robust inflammatory response, leading to the development of sepsis and associated complications, including disruptions in thermoregulation.
Thermoregulation During Sepsis: Insights from the CLP Model
The CLP model has provided valuable insights into the complex interplay between sepsis and thermoregulation. Researchers have observed that the body’s temperature response during sepsis can vary considerably, with some animals experiencing fever and others developing hypothermia. These temperature fluctuations are believed to be influenced by a variety of factors, including the severity of the infection, the individual’s immune response, and the activation of specific thermoregulatory pathways.
Fever and Hypothermia in Sepsis
In the early stages of sepsis, the body’s initial response is often characterized by a fever, as the immune system mobilizes to fight the infection. This fever response is mediated by the release of inflammatory mediators, such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α). These cytokines act on the hypothalamus, the brain’s thermoregulatory center, to raise the body’s set point for temperature control.
However, as sepsis progresses and the inflammatory response becomes dysregulated, the body may transition from a febrile state to a hypothermic one. Hypothermia in sepsis is thought to be a consequence of various factors, including vasodilation, decreased metabolic rate, and impaired shivering response. The underlying mechanisms behind this shift from fever to hypothermia in sepsis are not fully understood, but they are believed to involve complex interactions between the immune system, the nervous system, and the body’s thermoregulatory mechanisms.
The Role of the Autonomic Nervous System
The autonomic nervous system plays a crucial role in regulating body temperature during sepsis. The sympathetic nervous system, responsible for the “fight-or-flight” response, is often hyperactivated in sepsis. This can lead to excessive vasodilation, which can cause a drop in peripheral resistance and a decline in cardiac output. These circulatory changes can impair the body’s ability to maintain a stable core temperature, contributing to the development of hypothermia.
Conversely, the parasympathetic nervous system, which is associated with the “rest-and-digest” response, may become suppressed during sepsis. This imbalance between the sympathetic and parasympathetic systems can further disrupt the body’s thermoregulatory mechanisms, exacerbating the temperature fluctuations observed in septic patients.
The Impact of Thermoregulatory Dysfunction on Survival
The disruption of thermoregulation during sepsis can have significant consequences for patient outcomes. Fever and hypothermia have both been associated with increased mortality in septic patients. Fever, if left unchecked, can lead to further inflammatory cascades, organ dysfunction, and dehydration, while hypothermia can compromise the body’s ability to mount an effective immune response and can also contribute to cardiovascular instability.
The CLP model has provided valuable insights into the relationship between thermoregulatory dysfunction and survival in sepsis. Studies using the CLP model have demonstrated that the degree of temperature fluctuations, as well as the timing and duration of these changes, can significantly impact survival. For example, animals that develop persistent hypothermia during the course of sepsis tend to have a poorer prognosis compared to those that are able to maintain a more stable body temperature.
Therapeutic Interventions and Thermoregulation
Given the critical role of thermoregulation in sepsis, researchers have explored various therapeutic interventions that aim to restore and maintain a stable body temperature in septic patients. These strategies range from pharmacological approaches to more targeted interventions.
Pharmacological Interventions
One approach involves the use of antipyretic drugs, such as acetaminophen or ibuprofen, to manage fever in septic patients. These medications work by inhibiting the production of prostaglandins, which are key mediators of the fever response. While the use of antipyretics has been a standard practice in the management of sepsis, the evidence regarding their impact on patient outcomes has been mixed.
Another pharmacological intervention involves the use of vasopressors, such as norepinephrine or vasopressin, to counteract the vasodilation associated with sepsis-induced hypothermia. These drugs can help restore peripheral vascular tone and improve cardiovascular stability, which may in turn support the body’s thermoregulatory mechanisms.
Targeted Interventions
In addition to pharmacological approaches, researchers have explored more targeted interventions to address thermoregulatory dysfunction in sepsis. One such strategy is the use of external warming devices, such as heated blankets or warming pads, to actively maintain the patient’s body temperature within a physiologically normal range. These interventions aim to prevent the development of hypothermia and support the body’s own thermoregulatory mechanisms.
Another approach involves the use of targeted temperature management, also known as “controlled cooling” or “therapeutic hypothermia.” In this approach, the body’s temperature is intentionally lowered, typically to a range of 32-34°C (90-93°F), in an effort to mitigate the detrimental effects of the inflammatory response and improve survival. The rationale behind this strategy is that controlled hypothermia can reduce metabolic rate, decrease the production of reactive oxygen species, and modulate the immune response, potentially leading to better patient outcomes.
The CLP model has been instrumental in evaluating the efficacy of these targeted interventions. Studies using the CLP model have provided valuable insights into the optimal timing, duration, and degree of temperature manipulation required to achieve the best outcomes in septic animals. These findings have informed the design and implementation of clinical trials exploring the use of targeted temperature management in human sepsis patients.
Conclusion
The cecal ligation and puncture (CLP) model has been a valuable tool in elucidating the complex relationship between sepsis, thermoregulation, and survival. This animal model has provided a deeper understanding of the mechanisms underlying the temperature fluctuations observed in septic patients, as well as the impact of these thermoregulatory disturbances on clinical outcomes.
By leveraging the insights gained from the CLP model, researchers and clinicians can work towards developing more effective strategies for the management of sepsis. This may involve the use of targeted pharmacological interventions, external warming devices, or controlled temperature management approaches to restore and maintain a stable body temperature in septic patients.
Ultimately, the goal is to optimize the body’s thermoregulatory mechanisms and support the overall immune response, thereby improving the chances of survival for those battling the devastating effects of sepsis. As we continue to explore the intricacies of this condition, the CLP model will remain a valuable tool in advancing our understanding and shaping the future of sepsis management.

