Introduction
Dental health is a critical aspect of overall well-being, and the team at Station Road Dental Aldergrove is dedicated to providing comprehensive care to our patients. In this article, we’ll delve into the intricacies of a rare medical condition that can have significant implications for dental treatment: acute pancreatitis following a complex cardiac surgery.
Acute Pancreatitis: A Rare Complication
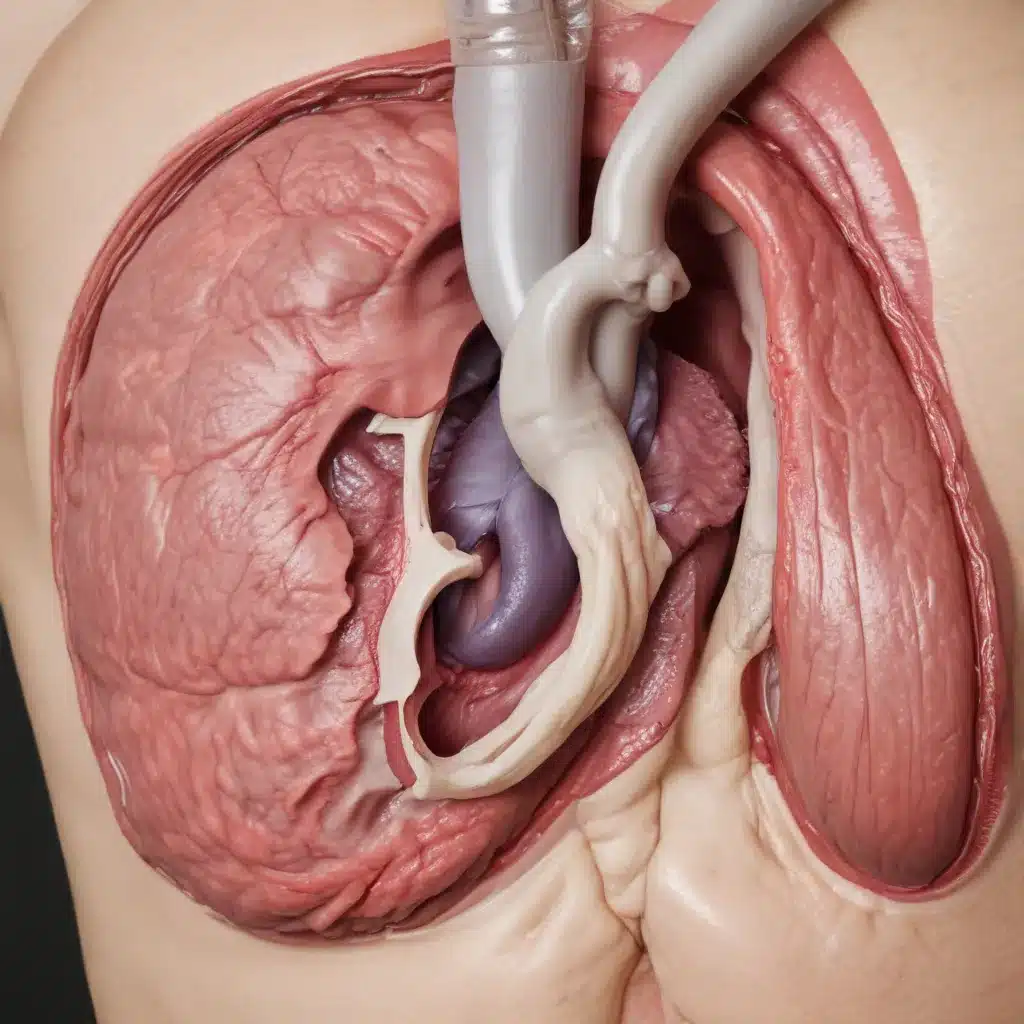
Acute pancreatitis is an inflammation of the pancreas that can occur due to a variety of factors, including gallstones, alcohol abuse, and, in some cases, as a complication of major surgical procedures. In a recent case study published in the Journal of Cardiothoracic Surgery, researchers reported on a patient who developed acute pancreatitis following a double cardiac valve replacement surgery.
The case report, titled “Acute pancreatitis after double cardiac valve replacement: a case report,” highlights the importance of understanding the potential risks associated with certain medical conditions and how they can impact dental care. As a dental health expert, it is crucial to be aware of these types of complications and their implications for patient management.
Understanding Acute Pancreatitis
Acute pancreatitis is a sudden and severe inflammation of the pancreas, a vital organ located behind the stomach. The pancreas plays a crucial role in digestion, producing enzymes that help break down food, as well as hormones like insulin that regulate blood sugar levels.
When the pancreas becomes inflamed, it can cause intense abdominal pain, nausea, vomiting, and other symptoms. In severe cases, acute pancreatitis can lead to complications, such as organ failure or the development of fluid collections or abscesses in the abdomen.
The exact mechanism by which acute pancreatitis can occur after cardiac surgery is not fully understood, but it is believed to involve a combination of factors, including:
- Reduced blood flow to the pancreas: The stress of the surgical procedure and the use of cardiopulmonary bypass can temporarily reduce blood flow to the pancreas, leading to ischemia (lack of oxygen) and inflammation.
- Release of inflammatory mediators: The body’s inflammatory response to the surgical trauma can trigger the release of various cytokines and other mediators, which can further contribute to pancreatic inflammation.
- Medication side effects: Some of the medications used in the perioperative period, such as certain antibiotics or pain relievers, may potentially contribute to the development of acute pancreatitis in susceptible individuals.
Dental Considerations for Patients with Acute Pancreatitis
The development of acute pancreatitis in a patient who has undergone a major cardiac surgery can have significant implications for their dental care. As a dental health expert, it is crucial to understand the potential risks and considerations when providing treatment to these individuals.
Timing of Dental Procedures
Patients recovering from acute pancreatitis may need to postpone non-essential dental procedures until their condition has stabilized and the inflammation has subsided. Performing dental work during the acute phase of the illness could potentially exacerbate the pancreatitis or lead to other complications.
It is generally recommended to wait at least 4-6 weeks after the onset of acute pancreatitis before resuming routine dental care, such as prophylaxis (routine cleaning) or restorative procedures. In more severe cases, the waiting period may need to be longer, depending on the patient’s clinical course and the guidance of their medical team.
Pain Management and Medication Interactions
Patients with acute pancreatitis may experience significant abdominal pain, which can complicate the management of dental pain or discomfort. Dental professionals must be cautious when prescribing pain medications, as some common analgesics (such as non-steroidal anti-inflammatory drugs) can potentially exacerbate pancreatic inflammation.
It is essential to carefully review the patient’s medication regimen, including any medications prescribed for the management of their acute pancreatitis, to avoid potentially harmful drug interactions or adverse effects. Consultation with the patient’s medical team may be necessary to determine the safest and most effective pain management strategies.
Infection Control and Antibiotic Considerations
Acute pancreatitis can lead to a weakened immune system and an increased risk of infection. As a result, dental professionals must be particularly vigilant in maintaining strict infection control protocols when providing care to these patients.
In some cases, the use of prophylactic antibiotics may be recommended, especially when performing invasive dental procedures, such as extractions or endodontic treatments. The specific antibiotic regimen should be determined in collaboration with the patient’s medical team, taking into account the patient’s current condition, any ongoing infections, and the potential for antibiotic interactions.
Nutritional Considerations
Patients with acute pancreatitis may experience difficulties with food intake and digestion, which can impact their overall nutritional status. This can have implications for wound healing and the body’s ability to respond to dental procedures.
Dental professionals should be aware of the patient’s nutritional status and work closely with the medical team to ensure that the patient is receiving adequate nutrition, either through dietary modifications or supplementation, as needed. This may involve collaboration with a registered dietitian or nutritionist.
Case Report: Acute Pancreatitis after Cardiac Surgery
The case report published in the Journal of Cardiothoracic Surgery describes a 72-year-old patient who developed acute pancreatitis following a double cardiac valve replacement surgery.
The patient, who had a history of rheumatic heart disease, underwent a successful surgical procedure to replace both the mitral and aortic valves. However, in the postoperative period, the patient began experiencing severe abdominal pain, nausea, and vomiting.
Diagnostic tests, including CT scans and laboratory analyses, confirmed the diagnosis of acute pancreatitis. The patient was immediately transferred to the intensive care unit and received supportive care, including fluid resuscitation, pain management, and close monitoring.
Over the course of several weeks, the patient’s condition gradually improved, and the acute pancreatitis resolved. During this time, the patient’s dental care was postponed, and the dental team closely monitored the patient’s progress and coordinated with the medical team to ensure a safe and appropriate plan for resuming dental treatment.
This case highlights the importance of dental professionals being aware of the potential complications that can arise in patients with complex medical histories, such as those undergoing major cardiac surgeries. By understanding the risks and taking the necessary precautions, dental practitioners can help ensure the best possible outcomes for their patients.
Preventive Dental Care and Maintenance
While acute pancreatitis in the context of cardiac surgery is a rare occurrence, it is essential for dental professionals to recognize the importance of preventive dental care and maintenance for all patients, regardless of their medical history.
Regular dental examinations, professional cleanings, and oral hygiene instructions can help patients maintain good oral health and reduce the risk of dental emergencies or complications that may arise during periods of medical instability.
By encouraging patients to establish and maintain a consistent routine of preventive dental care, dental professionals can help mitigate the potential risks associated with acute pancreatitis or other medical conditions, and ensure that patients receive the necessary care to maintain their overall health and well-being.
Conclusion
The case report on acute pancreatitis following a double cardiac valve replacement surgery highlights the importance of dental professionals being aware of the potential complications that can arise in patients with complex medical histories. By understanding the risks, taking appropriate precautions, and working closely with the patient’s medical team, dental practitioners can help ensure the best possible outcomes for their patients.
At Station Road Dental Aldergrove, we are committed to providing comprehensive, compassionate, and evidence-based dental care to all of our patients. If you or a loved one have a complex medical condition and are in need of dental treatment, we encourage you to contact us to schedule a consultation. Our team of experienced professionals will work closely with you and your medical team to develop a personalized treatment plan that addresses your unique needs and concerns.

